Cardiac conditions with clinical patterns that represent myocardial infarctions and unstable angina fall into the category of ACS. Unstable angina, Non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) are the main classifications of ACS, diagnosed with the help of electrocardiograms (ECG) and blood tests. Devising a risk stratification method is possible only with in-vivo evaluation of the vulnerable plaque. Advanced medical imaging techniques such as intravascular ultrasound (IVUS), angioplasty surgery and optical coherence tomography (OCT) helps in assessing the pathophysiology of plaque formation, erosion and rupture. Treatment of acute coronary artery syndrome mainly involves medical therapy and revascularization procedures. Anti-ischemic agents, anti-platelet agents and anti coagulants are the standard pharmacological treatment options prescribed by physicians. Revascularization procedures include percutaneous coronary intervention (PCI) and Coronary Artery Bypass Graft (CABG). Fractional Flow Reserve guided percutaneous intervention helps the cardiologist determine whether to treat the lesions with stenting or medical therapy. The patient’s cardiac health, risk score and several other factors are taken into consideration to choose between and bypass and angioplasty surgery.
Continuing Education
Get Cardiology related Articles, Journals, Videos and more details at Radcliffe Cardiology site.
Online Cardiovascular Disease
Go to read Online Cardiovascular Disease relarted articles via atrial fibrillation association afa.
Cardiology Mayo Clinic
Cardiology Mayo Clinic provides informative info about cardiology at RC site.
Cardiovascular Research Foundation
Free and register PDF and journales available at here!!!
Cardiology Video
Arrange seminar and online video conference by expert cardiologist, Visit at site.
Tuesday, 30 December 2014
Fractional Flow Reserve Measurements in the Management of Acute Coronary Artery Syndrome
By Unknown02:56Acute Coronary Artery Syndrome, Angioplasty Surgery, Fractional Flow ReserveNo comments

Cardiovascular diseases are a leading cause of mortality and morbidity around the world. Coronary artery disease (CAD), commonly known as heart disease is the end product of atherosclerotic plaque formation. High blood pressure, smoking or high cholesterol levels are some of the risk factors that worsen the atherosclerotic condition. Stable angina and acute coronary artery syndrome (ACS) are the two main sub categories of clinical patterns produced by CAD. Coronary arteries that harden up due to the atherosclerosis limit the blood supply to the heart, thereby damaging the myocardial tissues (ischemia). Rupture of a vulnerable plaque causes occlusive intracoronary thrombus which further leads to the complete obstruction of blood supply, resulting in unstable angina or myocardial infarctions (heart attacks). Even though chest pain (angina) and discomfort are considered as the common symptoms of CAD, it is essential to perform the diagnostic procedures in order to distinguish patients with Acute Coronary artery syndrome. Prompt medical attention and diagnosis is crucial for treating the ACS patients as it is the major cause of infarctions.
Cardiac conditions with clinical patterns that represent myocardial infarctions and unstable angina fall into the category of ACS. Unstable angina, Non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) are the main classifications of ACS, diagnosed with the help of electrocardiograms (ECG) and blood tests. Devising a risk stratification method is possible only with in-vivo evaluation of the vulnerable plaque. Advanced medical imaging techniques such as intravascular ultrasound (IVUS), angioplasty surgery and optical coherence tomography (OCT) helps in assessing the pathophysiology of plaque formation, erosion and rupture. Treatment of acute coronary artery syndrome mainly involves medical therapy and revascularization procedures. Anti-ischemic agents, anti-platelet agents and anti coagulants are the standard pharmacological treatment options prescribed by physicians. Revascularization procedures include percutaneous coronary intervention (PCI) and Coronary Artery Bypass Graft (CABG). Fractional Flow Reserve guided percutaneous intervention helps the cardiologist determine whether to treat the lesions with stenting or medical therapy. The patient’s cardiac health, risk score and several other factors are taken into consideration to choose between and bypass and angioplasty surgery.
Cardiac conditions with clinical patterns that represent myocardial infarctions and unstable angina fall into the category of ACS. Unstable angina, Non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) are the main classifications of ACS, diagnosed with the help of electrocardiograms (ECG) and blood tests. Devising a risk stratification method is possible only with in-vivo evaluation of the vulnerable plaque. Advanced medical imaging techniques such as intravascular ultrasound (IVUS), angioplasty surgery and optical coherence tomography (OCT) helps in assessing the pathophysiology of plaque formation, erosion and rupture. Treatment of acute coronary artery syndrome mainly involves medical therapy and revascularization procedures. Anti-ischemic agents, anti-platelet agents and anti coagulants are the standard pharmacological treatment options prescribed by physicians. Revascularization procedures include percutaneous coronary intervention (PCI) and Coronary Artery Bypass Graft (CABG). Fractional Flow Reserve guided percutaneous intervention helps the cardiologist determine whether to treat the lesions with stenting or medical therapy. The patient’s cardiac health, risk score and several other factors are taken into consideration to choose between and bypass and angioplasty surgery.
Huge advancements have been made in evaluating the extent and severity of culprit lesions of ACS which helps in the effective management of the condition. Novel antiplatelet drugs, pressure wire guided percutaneous interventions, fractional flow reserve and drug eluting stent implantations are some of the noteworthy achievements.
Monday, 22 December 2014
Management of Atrial Fibrillation
By Unknown22:33Blood Flow Blood Pressure, Paroxysmal Atrial Fibrillation, Surgical PocketNo comments

The human heart is a muscular pump which beats as a result of electrical impulses produced by a special group of cells in the heart that have the ability to generate electrical activity on their own. Any abnormalities in the heart rate or rhythm can be considered to be a fault in the electrical conduction system of the heart. If the heart rate remains constantly slower (bradycardia) or faster (tachycardia) with irregular rhythm, then it may be a heart condition called arrhythmia. Diagnosis of arrhythmia involves collecting information about symptoms, evaluating medical history and a physical exam. Electrocardiogram, cardio monitoring and blood flow blood pressure measurements are some of the diagnostic tests, blood pressure and procedures performed to identify the underlying cause of abnormal heart rhythms.
Atrial fibrillation
or A-fib (AF) is a type of arrhythmia that happens when the electrical signals are not only generated from sinus node, but are also generated from different places in and around the right atrium. When the atrioventricular node (AV node) – the electrical relay station between the upp and lower chambers of the heart-- is flooded with multiple erratic signals it leads to twitching of atria and desynchronised contractions of heart chambers. There are mainly three types of atrial fibrillation - Paroxysmal Atrial Fibrillation, Persistent Atrial Fibrillation and Permanent Atrial Fibrillation. Whenever the A-fib lasts from a few seconds to about a week, it is termed as Paroxysmal Atrial Fibrillation and when the A-fib episode continues for more than seven days, the condition is called persistent atrial fibrillation. When the abnormal heart rhythm persists all the time, it is called permanent atrial fibrillation. Both the paroxysmal and persistent AF can progress to permanent AF over a period of time, which is why it is highly recommended to seek treatment as early as possible.
AF episodes cause a disruption in the blood flow thereby increasing the likelihood of blood clot formation. That is why risk of acute cardiovascular events and strokes are higher among people with atrial fibrillation. Treatment of Afib aims in cutting down the risk of blood clot formation and restoring the normal heart rhythm. Medical therapy using anticoagulants and electrical interventions are performed to treat this heart condition. Electro cardioversion, catheter ablation and surgical pocket maze are the standard procedures opted by the cardiologists to treat arrhythmias. In some cases, ablate and pace approach is recommended. During this procedure, the AV node is destroyed and an artificial pacemaker is placed in the surgical pocket of the chest to ensure a regular backup rhythm. Choosing between pharmacological treatment and ablation procedures always comes down to factors such as degree of AF episodes, cardio health and evaluation of surgical complications.
AF episodes cause a disruption in the blood flow thereby increasing the likelihood of blood clot formation. That is why risk of acute cardiovascular events and strokes are higher among people with atrial fibrillation. Treatment of Afib aims in cutting down the risk of blood clot formation and restoring the normal heart rhythm. Medical therapy using anticoagulants and electrical interventions are performed to treat this heart condition. Electro cardioversion, catheter ablation and surgical pocket maze are the standard procedures opted by the cardiologists to treat arrhythmias. In some cases, ablate and pace approach is recommended. During this procedure, the AV node is destroyed and an artificial pacemaker is placed in the surgical pocket of the chest to ensure a regular backup rhythm. Choosing between pharmacological treatment and ablation procedures always comes down to factors such as degree of AF episodes, cardio health and evaluation of surgical complications.
Monday, 15 December 2014
Recent Advances in Cardiac Electrophysiology
Cardiology,
being a prime medical speciality has always been in the forefront of inventing new diagnostic techniques, medical therapies, interventional procedures, medical imaging, continuous monitoring systems and more. Among the many recent
advancements, leadless pacemaker and thermocool smarttouch catheter offer a promising approach in treating problems with the heart's electrical conduction system.
Thermocool Smarttouch catheter: In a healthy heart, the electrical impulses are generated from the sinoatrial (SA) node which controls the speed or rhythm of beats. Any disruption or error in this conduction process leads to arrhythmia resulting in either too fast heart rate or too slow heart rate. Cardiac ablation is a medical procedure that is often preferred by the physicians to treat arrhythmias for those patients who don’t respond positively to drug therapy. During this catheterization procedure, continuous monitoring and radio frequency energy is used to scar the sources of abnormal heart rhythms. However, the procedure can fail sometimes because of inadequate lesion formation. Thermocool smarttouch catheter – an innovative discovery in electrophysiology focuses to resolve this drawback as it is integrated with contact-force sensing technology to provide detailed evaluation of catheter-to-myocardial contact force and catheter stability. This will guide the physicians to apply the stable force to the tissues without any risk of injury or complications.
Leadless pacemaker:Cardiologists have been recommending pacemakers for most of the patients suffering with bradyarrhythmias (too slow heart beat) or heart block. Taking over the job of the SA node, this electrical device restores electrical conduction through the heart. A surgical incision has to be made in the chest to place the pacemaker. Leads are connected to it which acts as a conduit for the delivery of electrical pulses that stimulate the heart functioning. However, acute and chronic complications arise whenever the surgical pocket is infected or leads are displaced. That is why leadless pacing technologies have gained
immense interest in the field of cardiology. Self-contained leadless pacemakers that are different from its conventional counterparts don’t require any surgical incision or leads and can be placed through a catheterization procedure. Trial results and findings support the use of this less-invasive pacemaker technology.
It can be said that the future of interventional cardiology and electrophysiology looks bright and ensures to improve the quality of patient’s life.
Monday, 8 December 2014
Use of Drug-Eluting Stents during Percutaneous Coronary Intervention
By Unknown01:44Coronary Fractional Flow Reserve, Cre8, Percutaneous Coronary InterventionNo comments

Narrowing of arteries and obstruction in the blood supply to the heart may lead to major cardiovascular events such as ischemia, myocardial infarction (heart attack), stroke and more. Plaques that build-up in the coronary arteries can behave in different ways: a plaque that grows to certain size and stops, a plaque that eventually causes blockage or a plaque that suddenly ruptures causing a complete block of blood supply. Chest pain during exertion is a sign of stable plaque whereas heart attack or stroke occurs when there is a plaque rupture. Cardiologists will either opt for drug therapy or revascularization procedures - percutaneous coronary intervention and Coronary Artery bypass Grafting - depending on the diagnostic results of CAD patients.
Physicians often prefer a less invasive approach as it cuts down the complications and speeds up the recovery time. Percutaneous coronary intervention (PCI), also known as coronary angioplasty have become one of the most preferred coronary interventions because of its improved outcomes and dramatic reduction of major adverse cardiac events (MACE). The procedure mainly involves widening of the narrowed artery with an inflated balloon-tipped catheter thereby restoring the normal blood flow. However, in some cases it may be essential to perform a stenting procedure to keep the arteries open. An interventional cardiologist has to take the decision about whether or not to place the stents, based on angiographic data and fractional flow reserve measurements. Coronary Fractional Flow Reserve technique used during catheterization provides a lesion-specific index that guides the physician to decide the treatment approach. Stents are placed only when the measured FFR value is less than 0.75, otherwise the patient is prescribed with medical therapy.
The well-validated and threshold value provided by the coronary fractional flow reserve technique have become a standard and reliable way to demonstrate or exclude ischemia-inducing lesions. To return to the subject of stenting, two classes of stents namely Bare-metal stents (BMS) and Drug-Eluting Stents (DES) are available for PCI. DES has superseded the use of BMS as it prevents the formation of scar tissue thereby reducing the likelihood of restenosis to a greater extent. For instance, Cre8™ DES (a polymer-free DES coated with Amphilimus™) is a new step in DES technology that overcomes the polymer-associated complications and minimises the risk of thrombosis. The amphicilic carrier present in Cre8™ DES proposes a controlled and directed drug elution. Dramatic development of nanotechnology and DES technology offers a promising approach in developing a biocompatible stent that would completely eliminate restenosis and thrombosis in near future.
Wednesday, 3 December 2014
Why Diagnosis of Treatment Resistant Hypertension is Important?
By Unknown23:02Blood Flow Blood Pressure, Treatment Resistant Hypertension, Xper Flex CardioNo comments

It is a well known fact that heart diseases have been claiming the lives of people more than any other disease. Termed as Coronary Heart Disease, this cardiac condition leads to heart attack, stroke and other major cardiovascular events. Treatment of coronary heart disease mainly focuses on controlling the risk factors by making lifestyle changes and prescribing drug treatments. High blood pressure (hypertension) and high blood cholesterol levels are the biggest risk factors that need to be brought under control. Several studies, clinical trials and research findings have stated that patients with resistant hypertension are even at higher risk of cardiovascular morbidity, stroke and mortality. Treatment resistant hypertension is a medical condition when the blood pressure remains stubbornly above the target in spite of the use of a diuretic and at least two other medications; patients whose blood pressure is controlled by four or more medications can be termed as resistant to treatment.
Accurate diagnosis and effective use of multiple drug regimens is significant in order to tackle treatment resistant hypertension. The goal blood pressure is less than 140/90 mmHg and achieving this level is even more important among resistant hypertension patients as it is associated with worse cardiovascular events. Taking accurate measurements of blood flow blood pressure is substantial for confirming treatment resistance. Direct (invasive) and indirect (non-invasive) methods are available for measuring the blood pressure and blood flow. Direct method involves using intra-arterial catheter to puncture a blood vessel and taking measurements directly, whereas the non-invasive method is about measuring the arterial pressure indirectly with a manual sphygmomanometer or an automated oscillometric device.
Physicians often prefer the indirect method because it’s the ‘gold standard’ method for routine measurements and monitoring. However, the accuracy levels of indirect measurements are low when compared to the direct methods. That is why it is important to have a hemodynamic monitoring system especially during the invasive procedures. Xper Flex Cardio physiomonitoring system introduced by Philips Healthcare is an innovative step towards this direction. It not only displays the invasive blood pressure blood flow, but also Fractional Flow Reserve measurements, ECG, respiration and other vital signs. Xper Flex Cardio systems prove to be of great use in areas where hemodynamic cardiac monitoring is required. To return to the subject of treatment resistant hypertension, we can say that ruling out the pseudoresistance factors and identification of the true causes can help in devising an effective prevention and management strategy of this condition.
Wednesday, 26 November 2014
Why FFR-Guided Revascularization Strategy Is More Effective?
Coronary Artery Disease (CAD) or Coronary Heart disease is a serious heart condition that occurs as a result of atherosclerosis. Hardening or narrowing of the artery (stenosis) causes an obstruction in the blood flow to the heart which may lead to major cardiovascular events. When the heart muscle is starved of oxygen, it results in acute chest pain and discomfort (angina) whereas heart attack (myocardial infarction) is the outcome of a completely blocked blood flow through a coronary artery. Hence, it is important to diagnose and treat coronary heart disease as early as possible, as time plays a crucial role here. Plaque build-ups along the inner walls of blood vessels can cause blockage in either single or multiple coronary arteries. Multi vessel disease (MVD) or Multi vessel CAD is the condition where a major epicardial vessel is affected with 70% or greater stenosis and other major vessels are affected with 50% or greater stenosis.
Medical therapy, Percutaneous Coronary Intervention (angioplasty and stenting) and Coronary Artery Bypass Grafting (CABG) are the treatment options available for coronary heart disease. Interventional cardiologists used to rely on angiography results and other clinical information to detect the evidence of inducible ischemia and guide treatment decisions. Notwithstanding coronary angiography is considered as the gold standard for CAD evaluation, it has been recognised to have several limitations in assessing the functional significance of coronary lesions. In the case of multi vessel coronary disease, the decision-making is far more challenging as angiographic data tend to either overestimate or underestimate the functional severity of stenosis. Revascularization of non-ischemic lesions not only increases the treatment costs but also poses an increased risk for the CAD patient rather than offering any benefit. That is when the results published by the FAME (Fractional Flow Flow Reserve versus Angiography in Multivessel Evaluation) study gained substantial interest in the medical community. It demonstrated that FFR-guided PCI can ensure better outcomes when compared to the angiography-guided PCI.
Fractional Flow Reserve (FFR) measurements can be taken easily during the invasive procedure just before the stenting. A 0.75 cut-off value helps in differentiating between ischemic and non ischemic stenosis. Lesions with a FFR value of less than 0.75 needs drug-eluting stents (DES) while lesions with a FFR value greater than 0.80 should be treated with medical therapy. The FAME study results proved that routine measurements of FFR during PCI significantly reduced the occurrence of myocardial infarction (MI), combined end point of death and repeat revascularization. So it can be hypothesised that FFR measurements are helpful in guiding decisions regarding whether CABG, stenting or medical therapy would be the optimal approach for each CAD patient.
Monday, 24 November 2014
Why Timely Coronary Artery Disease Treatment is Crucial?
By Unknown00:18Coronary Artery Disease Treatment, Coronary Artery Stenosis, Index of Microvascular Resistance2 comments

Heart muscle needs oxygen and nutrient rich blood to function properly and it is supplied by coronary arteries. When healthy, the coronary arteries remain strong, elastic and flexible which ensures the blood flow without any restrictions. However, the arterial health is compromised in some situations because of an underlying pathologic process called atherosclerosis which results in the thickening, loss of elasticity and calcification of coronary arteries. So build up of plaques in the coronary arteries coronary artery stenosis obstructs the blood flow to the heart, thereby weakening or damaging the heart muscles and this condition is termed as coronary heart disease or coronary artery stenosis disease (CAD). Whenever there is a partial blockage in blood supply, it leads to angina (chest pain or discomfort), while a complete blockage of blood flow causes myocardial infarction (heart attack).
Coronary Artery Disease treatment mainly includes medications, procedures and surgeries. Even some lifestyle changes can improve the quality of life. Medications are prescribed to treat the risk factors such as blood pressures, diabetes or high cholesterol levels so that it prevents the CAD from getting worse. Surgical options include angioplasty and stenting (Percutaneous Coronary Intervention) or coronary artery disease treatment or Bypass Grafting (CABG). Depending on the severity of coronary lesions, an appropriate treatment plan is chosen by the cardiologist. Several advanced catheterization procedures and imaging techniques guide the interventional cardiologists to assess the physiological significance of lesions. Angiography, Fractional Flow Reserve (FFR), Intra Vascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT) are some of the indispensable tools used in the catheterization laboratory.
Another heart disease that has gained considerable interest in the medical community is coronary microvascular disease (CMD), which particularly occurs in women. Damage or inflammation of the inner walls of the heart’s tiny arteries is the cause of CMD. Though the presence of this dysfunction can have prognostic implications in many heart vv diseases, there are no reliable standard tests available to detect this micrhovascular disease. Diagnostic techniques developed for CAD can’t be used to assess the microvasculature of the myocardium. For now, index of microvascular resistance (IMR) is a method to investigate the microvascular integrity and functional status of micro circulation. So, FFR and IMR measurements taken simultaneously during the catheterization can help in assessing the coronary artery disease and coronary microvascular resistance disease.
Thursday, 20 November 2014
Stenting and Bypass Surgery for Patients with Left Main Coronary Artery Disease
By Unknown22:00Coronary Arterial Stenosis, Left Main Coronary Artery (LMCA), Optical Coherence Tomography (OCT)No comments

The heart is a fist-sized powerhouse that pumps oxygen and nutrient-rich blood throughout the body to keep us alive. Aorta that bifurcate into two major coronary arteries – Left Main Coronary Artery (LMCA) and Right Coronary Artery (RCA) supply blood to the heart tissues keeping them nourished so that they can function perfectly. Left Coronary Artery also known as Left main stem coronary artery (LMS) branches into Left Anterior Descending Artery (LAD) and Left Circumflex Artery that supplies the left side of the heart muscles and front of the septum with blood. While the Right Coronary Artery divides into the Right Marginal Artery and Posterior Descending Artery which supplies blood to the right side of the heart and sinoatrial nodes. Hence, any blockage in the coronary arteries will disrupt or cut off the blood flow to the heart muscles (myocardium), resulting in its damage or death.
Plaque that builds up in the coronary arteries as a result of atherosclerotic condition is the major cause of restricted blood flow. Coronary arterial stenosis of greater than or equal to 50% narrowing is associated with multivessel disease and is termed as the significant left main disease (LMD). Patients with coronary heart disease often suffer from severe chest pain and discomfort as the heart becomes starved of oxygen and nutrients. In some cases, whenever there is a clogging in the right or left main coronary artery, the collateral vessels become active, and bypassing the blockage they serve as alternative conduits for blood flow. However, it is not a cure or standard medical care option to rely on the functioning of collateral arteries.
Medical therapy and surgical revascularization (Coronary Artery Bypass Graft Surgery and Percutaneous Coronary Intervention) are the main options available for treating coronary arterial stenosis. Medical therapy was not proven beneficial for treating LMD as the survival rates were far below. Performing bare-metal stenting often ended up in higher restenosis rates, acute thrombosis and repeat revascularization. Hence, Bypass surgery (CABG) turned out to be the standard of care for left main disease as it improves the likelihood of survival.
However, advancements in catheterization and medical imaging techniques such as FFR and Optical Coherence Tomography (OCT) have led to the resurgence of interest in Percutaneous coronary Intervention (PCI). Providing a detailed and clear visualization of coronary morphology, OCT has evolved as an indispensable tool for developing new types of coronary stents. Optical Coherence Tomography when used as a guide for coronary interventions ensures better outcomes. Even though, CABG remains to be the superior choice for treating left main CAD, cardiologists hope that the ongoing studies and trials may bring more light into the role of percutaneous approach in near future.
Monday, 17 November 2014
Treatment of Coronary Artery Stenosis
By Unknown22:17Bifurcation Lesions, Coronary Artery Stenosis, Coronary Heart Disease SymptomsNo comments

We have been hearing a lot about the rapid advancements and changes in the field of medical technology ranging from patient registration to data assessment and diagnostic methods to surgical procedures. Yet, some diseases continue to remain as a dreadful term for us; heart disease is a case in point. Coronary Heart Disease (CAD) also known as Coronary Artery Disease (CAD) is the most common type of heart disease that kills more people than any other disease across the world. The main cause of CAD is atherosclerosis (hardening of arteries). Build-up of calcium and cholesterol on the walls of coronary arteries cut down the blood supply to the heart muscles, thereby leading into cardiac ischemia or myocardial infarction (heart attack) among CAD patients.
Severe chest pain or discomfort, also termed as angina pectoris is one of the major coronary heart disease symptoms. The pain can be localised to shoulders, arms, neck, jaw or back. Though, in some cases people also experience nausea, shortness of breath and dizziness. The sensation of discomfort experienced during myocardial ischemia or myocardial infarction develops as a result of coronary artery stenosis. As the degree of coronary artery stenosis increases, myocardial blood flow is reduced resulting in severe chest pain.
Treatment plans differ according to the types of angina, which includes stable angina, unstable angina (UA), variant angina and microvascular angina. When stable angina follows a regular pattern, UA typically occurs when a person is at rest which demonstrates its highest unpredictability and risky nature. On the other hand, variant angina is a rare kind induced due to spasm in the coronary artery and can be treated with medical therapy. Severe pain persists for a long time when it comes to microvascular angina. Patients admitted with coronary heart disease symptoms are advised to undergo different laboratory tests and imaging studies to devise a treatment plan.
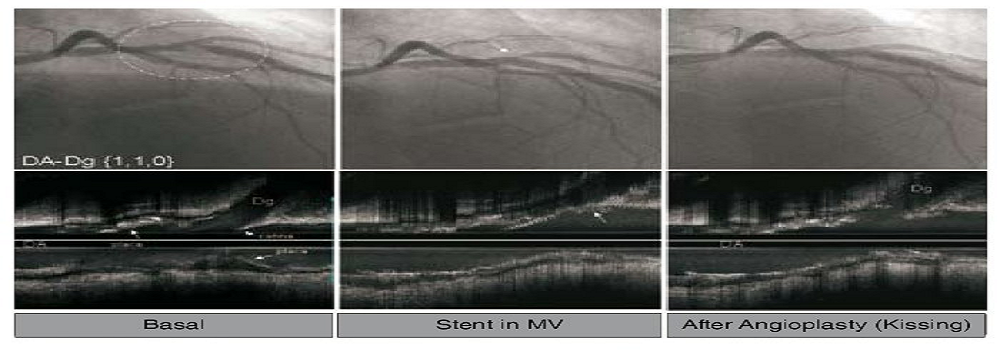
Surgical intervention or medical therapy is the preferred treatment approach to tackle coronary artery stenosis. However, interventional cardiologists find it challenging to deal with coronary bifurcation lesions (a lesion in the parent coronary artery very close or involving a significant side branch) that increases the procedural complexity. An optimal surgical or medical approach for managing coronary artery bifurcation lesions is still on debate as it involves restoring lumen of both the vessels. Time is the main factor in managing angina; hence it is essential to make a quick and safe decision based on the results.
Monday, 10 November 2014
Fractional Flow Reserve Measurement and Optical Coherence Tomography in Guiding Coronary Interventions
By Unknown01:58Fractional Flow Reserve Measurement, Multivessel Disease, Optical Coherence Tomography (OCT)No comments

Blockage of oxygen-rich blood supply to the heart due to the plaque build-up in coronary arteries is the primary cause for heart attacks. Termed as Coronary Artery Disease (CAD), this heart problem occurs due to a condition called atherosclerosis. In some cases, plaque build-up is not just limited within a single epicardial vessel but to multiple vessels known as Multi vessel CAD or coronary multivessel disease. If defined in medical terms - "a condition where 70% or greater stenosis is affected in at least one major epicardial vessel and 50% or greater stenosis is affected in at least other major vessels".
Though coronary angiography has been considered as the ‘gold standard’ for diagnosing ischemic heart conditions, it has many limitations. It often failed in providing comprehensive and accurate information about the physiological significance of lesions. That is when the well-validated Fractional Flow Reserve measurement came into the limelight. Performed along with the cardiac angiogram, it has been proved as a safe and reliable diagnostic tool to differentiate between ischemic and non-ischemic stenosis.
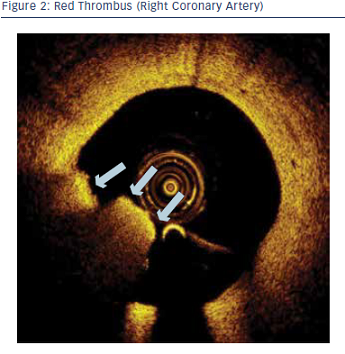
On the other hand, medical imaging techniques such as Intra Vascular Ultra Sound (IVUS) and Optical Coherence Tomography (OCT) have found a place in interventional cardiology. Functional severity of stenosis, plaque morphology and intraluminal coronary dimensions are some of the many features that can be assessed with IVUS. Whereas, OCT is slightly more efficient than the IVUS technique as it offers microscopic visualization of ten-times higher resolution. Advanced Optical Coherence Tomography technique renders clear and detailed pathophysiology of atherosclerotic plaque.
In terms of treatment choices for multivessel diseases, we presently have surgical management and medical therapy. Revascularization methods include Percutaneous Coronary Intervention (PCI) or angioplasty and Coronary Artery Bypass Graft (CABG) or bypass surgery. Reliable Fractional Flow Reserve Measurement value along with angiographic data helps physicians decide between PCI and medical therapy for single vessel CAD. Negating the need of repeated revascularization and relieving the likelihood of angina to a greater extent, CABG appears to be a superior choice over PCI when it is concerns treating multivessel disease. However, with the advancements in catheterization, medical imaging and stenting techniques, physicians are shifting away from the aggressive bypass surgical procedures and opting for less-invasive percutaneous treatments that ensure favourable long-term outcome. Yet, the optical treatment strategy for multi vessel CAD remains a controversial topic.
Wednesday, 15 October 2014
Cardiology Diseases, Disorders and Syndromes
All over the world, the death rate continues to increase as a restul of cardiology diseases. It is one of the critical issues in the medical world. Researchers and experts continue to innovate new technology, accessories and infrastructures, to help the increasing number of patients with cardiology diseases. Some common heart diseases and conditions include high cholesterol, Heart Failure, Atrial Fibrillation, Coronary Artery Disease, Mitral Valve Prolapse Syndrome. To provide better medical treatment to patients and to find new ways of treating such diseases, renowned cardiologists and experts organize conferences and seminars and publish authentic reviewed articles and case reports in medical journals.
There are few heart surgeons who
have expertise in Endovascular Surgery. These doctors perform major surgeries accessing many regions of the patient’s body and they try to give new life to the patient. The review articles and practice guides on Endovascular Surgery help thousands of professionals acquire a thorough knowledge about the field. Whether a cardiology professional belongs to the USA, UK or any other country, the professional can learn a lot from the authentic journals. The journals found on radcliffecardiology.com are published three times annually and contain theoretical discussions about cardiovascular subjects.
An important area covered by these journals includes original research on Peripheral Stenting and satellite symposia proceedings about Peripheral Stenting. Before any of the articles or case reports are printed in the journals, the expert team members ensure the accuracy of the content. The experts are selected for their clinical expertise and they provide reviews. These journals and conferences are a great source of information for the cardiology fraternity across the world. Many professionals, clinicians and physicians acquire detailed knowledge about medical treatment and surgery on heart problems through these articles and research papers.
Sunday, 12 October 2014
Participate in the Cardiologist Education Conference
Doctors go through essential cardiologist education training for many years to learn about medicine and heart surgery before they become heart surgeons. But, the number of the doctors in comparison to patients is few. As the number of heart patients is growing, researchers and expert cardiologists are working hard to provide essential Cardiologist education to professionals and health-providers to close the gap in the ratio of expert heart doctors to patients. Cardiovascular disease killed 17.5 million people in 2012, that is 3 in every 10 deaths and this is expected to rise to 23.3 million by 2030.
Indeed cardiovascular disease is a major issue around the globe. All over the world, many organizations organize seminars and conferences so that they can develop new solutions for controlling the disease. There are institutions that give opportunities to renowned speakers to share their research work on Coronary Stenting in seminars. Also, authentic articles and journals on Coronary Stenting are published so that more doctors learn about the latest innovations in the medical field.
Indeed cardiovascular disease is a major issue around the globe. All over the world, many organizations organize seminars and conferences so that they can develop new solutions for controlling the disease. There are institutions that give opportunities to renowned speakers to share their research work on Coronary Stenting in seminars. Also, authentic articles and journals on Coronary Stenting are published so that more doctors learn about the latest innovations in the medical field.
With the help of reviewed articles and practice guidelines, many professionals gain knowledge of Drug-Eluting Balloon Angioplasty and get in touch with the latest information in their field. The practice guides, review articles and case reports are carefully checked by experts before being published in medical journals. Knowledge of Drug-Eluting Balloon Angioplasty experts share their views in the form of theoretical discussions and original research. The aim of publishing all such information in journals is to keep cardiologists up to date with recent research and guidelines and to successfully treat and manage as many heart patients as possible more quickly. The seminars and conferences provide intensive training forcardiologists and keep them updated about high-tech medical equipment and its usage.
Monday, 6 October 2014
Cardiology Conferences aim to educate professionals
Cardiovascular disease is the world’s biggest killer. An estimated 17.3 million people died from CVDs in 2008 and this is believed to increase to more than 23 million people in 2030. Controlling these numbers is thus a major challenge and why major institutions and universities around the globe are working tirelessly to find new treatments. They organize cardiology conferences for professionals to share and discuss innovations in the field and provide delegates with information about recent research so that they can learn new ways of treating heart patients. In the world cardiology conferences, renowned speakers and reputed authorities gather to share findings and trial results to help medical practitioners learn about new innovations in cardiology.
Thousands of health-providers participate in these international seminars and receive new insights from cardiology journals and articles. Experts on Embolic Protection share their views and explore how heart surgeons can use carotid angioplasty in patients to save many lives. Embolic Protection devices are used to remove debris from cardiovascular disease patients. These seminars provide wide and deep knowledge about the latest treatment through papers written by researchers and experts.
Above all, medical information centers work incessantly in innovating new and easy ways of treatment so that expenses and the surgery time can be reduced. There are many recognized experts who published their articles and papers on Fractional Flow Reserve (FFR). They spend years in research to find the Fractional Flow Reserve (FFR) technique for measuring the pressure difference in coronary catheterization. Some practitioners are slow to learn about advances in mediacal treatments for heart patients and they continue applying traditional techniques. In these cases, research papers, journals and provide them a thorough knowledge about recent treatments.
Monday, 29 September 2014
Is CABG getting safer?
By Unknown00:57Coronary artery bypass surgery – CABG, Endovascular Surgery, Heart StentingNo comments

Stroke is one of the most devastating complications after coronary artery bypass graft (CABG) surgery, entailing permanent disability, a 3–6 fold increased risk of mortality, an incremental hospital resource consumption and a longer length of hospital stay. Notwithstanding advances in surgical, anaesthetic and medical management across the last 10 years, the risk of stroke after coronary artery bypass graft (CABG) has not significantly declined, likely because an older and sicker population is now deemed suitable to undergo CABG.
Advances in endovascular surgery have meant that whilst traditional "open heart" procedure is still performed and often preferred in many situations, newer, less invasive techniques have been developed to bypass blocked coronary arteries. "Off-pump" procedures, in which the heart does not have to be stopped, were developed in the 1990's. Other endovascular surgery procedures, such as key-hole surgery (performed through very small incisions) and robotic procedures (performed with the aid of a moving mechanical device), increasingly are being used.
Risk stratification is of the utmost importance for identifying vulnerable patients. Specifically, pre-existing cerebrovascular disease and atherosclerosis of the ascending aorta are major determinants of the risk of peri-operative stroke, and should be always carefully scrutinised. RCTs and meta-analysis do not clearly support routine implementation of offpump CABG as a strategy to minimise the risk of stroke. Observational studies have suggested that anaortic approaches might reduce the risk of stroke compared with conventional CABG in patients with severe atherosclerosis of the ascending aorta. Further randomised controlled trials are warranted to confirm this hypothesis. Heart stenting is another option for treating patients with CABG. The clinical application of drug-eluting stents (DES) or coronary artery bypass grafting (CABG) for unprotected left main coronary artery disease (ULMCAD) is still controversial. The need for repeat revascularization is significantly lower with CABG, but the risk of stroke is significantly higher, a trade-off that must be taken into account when considering heart stenting for patients with advanced coronary disease.
Sunday, 21 September 2014
FFR-Guided PCI Using Contemporary Drug-Eluting
Fractional flow reserve (FFR)-guided drug-eluting stenting reduces death, myocardial infarction or urgent revascularisation, as compared to medical therapy in patients with stable coronary artery disease (CAD), according to the results of the FAME 2 trial presented at the European Society of Cardiology’s (ESC) Congress. Whilst percutaneous coronary intervention (PCI) has been performed for more than 30 years, its benefits in terms of 'hard endpoints' as compared to medical therapy (MT) have never been demonstrated in patients with stable CAD. In patients with stable CAD the rate of death, MI, or urgent revascularisation at two years in those treated with FFR-guided PCI using contemporary drug-eluting stenting was less than half of what it was in patients treated with MT alone, in this study.
In another recent study, these stents were compared to the more traditional bare metal stents. Presented at the American College of Cardiology's 63rd Annual Scientific Session, the study showed Medtronic's Endeavor zotarolimus-eluting stent is associated with a lower risk of major cardiovascular events at one year compared to bare metal stents among a patient population normally excluded from treatment with drug-eluting stents.
Advances in the design and technology of medical devices and delivery systems, coupled with demand for alternative non-surgical therapies for common medical problems, including heart failure, have led to an increase in the volume, variety and complexity of non-coronary cardiac interventional procedures performed. The greater complexity of these newer procedures, particularly those involving heart valve intervention, necessitates more sophisticated and exacting imaging techniques, both to facilitate appropriate case selection and
to provide procedural guidance, thus increasing the likelihood of successful outcome. Contemporary advances in echocardiography imaging techniques ensure these modalities are well suited to the imaging requirements of this exciting and expanding field of interventional cardiology. Realtime 3D imaging, made possible by the development of a full matrix transducer capable of acquiring pyramidal-shaped ultrasound data sets, has been a major advance in
transthoracic echocardiography (TTE) for examining patients with suspected heart failure.
Thursday, 11 September 2014
Cardiology Stem Cell Therapy Offers Cardiac Repair
Cardiology stem cell therapy offers great hope and is the topic of much discussion. Currently, basic research scientists and clinicians worldwide are investigating human embryonic cardiac stem cells, skeletal stem cells (myoblasts), adult bone marrow stem cells, cardiology stem cells and human umbilical cord stem cells for the treatment of patients with MIs and ischaemic cardiomyopathies.ÿWhilst important
progress is occurring in the use of stem cells for cardiac repair, the most optimal stem cell(s) for treatment of patients with infarcted myocardium is yet to be determined.
At present, there are no widely used stem cell therapies other than bone marrow transplant. Research is underway to develop various sources for stem cells and to apply them to heart disease and other conditions.
Another exciting area is the field of stenting. The introduction and widespread adoption of drug-eluting stents into routine clinical practice has seen tremendous changes in the practice of interventional cardiology. For a prolonged period, manufacturers have focused research on drugs and polymers that are the key to the prevention of in-stent restenosis. However, stent platform design and its clinical implications have now come back to the fore. Manufacturers and clinicians will have to work closely in partnership to makesure that stenting devices can provide excellent safety and long-term efficacyfor patients.
Cardiology associates should have a complete understanding of the design features of the devices that they are implanting. It is likely that LMS PCI and the treatment
of large vessel bifurcations will become a mainstream application of PCI over the forthcoming years and manufacturers may need to consider producing dedicated platforms for the treatment of these vessels. As more patients with multivessel disease are treated greater attention will also need to be placed on longer-term outcomes in more demanding clinical settings, an area aboutwhich cardiology associates will need to be kept up-to-date.
The risks of latent stent fracture may assume a more prominent role in clinical studies in future. Ultimately, as the clinical practice of PCI continues to evolve, manufacturers and clinicians will have to work closely in partnership to make sure that the stenting devices that are implanted can provide excellent safety and long-term efficacy for patients. The importance of stent design has been re-emphasised and is likely to become increasingly relevant in future, where the patient and lesion being treated are likely to mandate very careful selection of the stents that are deployed in each individual setting. The focus should be shifted away from producing ever more deliverable stent platforms and should be moved back to the fundamental properties of what the device has been built to achieve.
Thursday, 4 September 2014
How heart stents (and their relatives) have gone from strength to strength
Heart stents have come a long way since doctors first started using balloon angioplasty to treat narrowed coronary arteries. During this procedure, a very thin, long, balloon-tipped tube (catheter), is inserted into an artery in either the groin or arm and is moved to the site of the blockage with help from an X-ray. The balloon at the tip of the catheter is then inflated to compress the blockage and restore blood flow, and is then deflated to allow the catheter and balloon to be removed. In some cases, these heart stents aren’t enough to prevent collapse of the coronary arteries after the balloon is deflated and restenosis can also be a side-effect. This led to the development of small stents which could be mounted on the balloon section of the catheter. These stents then expand when the balloon is inflated, lock into place, and form a permanent scaffold to hold the coronary artery open after the balloon is deflated and removed.
Carotid artery stenting (CAS) has increasingly assumed an important role in the management of significant carotid artery stenosis, and recent recommendations (by the UK National Institute for Health and Clinical Excellence (NICE) and the American Heart Association (AHA) suggest that it is a viable alternative to carotid endarterectomy (CEA) for standard-risk populations. There is a consensus among experts suggesting that embolic protection devices (EPDs) can reduce the risk of stroke during CAS. These recommendations are supported by an early meta-analysis. Embolic protectiondevices can be divided into three distinct types based on their mechanism of operation: distal occlusion aspiration devices, distal filters and proximal occlusion aspiration devices.
Devices aside, cardiology training in carotid artery stenting is imperative in terms of technical success rates, as it is in any new or technically challenging procedure. In a report which examined four groups of 50 patients, the authors observed a significant increase in technical success rate after 50 procedures and a concomitant reduction in total procedural time and contrast volume used, demonstrating a clear benefit of cardiology training.
Monday, 1 September 2014
Is CABG getting safer?
Stroke is one of the most devastating complications after coronary artery bypass graft (CABG) surgery, entailing permanent disability, a 3–6 fold increased risk of mortality, an incremental hospital resource consumption and a longer length of hospital stay. Notwithstanding advances in surgical, anaesthetic and medical management across the last 10 years, the risk of stroke after coronary artery bypass graft(CABG) has not significantly declined, likely because an older and sicker population is now deemed suitable to undergo CABG.
Advances in endovascular surgery have meant that whilst traditional "open heart" procedure is still performed and often preferred in many situations, newer, less invasive techniques have been developed to bypass blocked coronary arteries. "Off-pump" procedures, in which the heart does not have to be stopped, were developed in the 1990's. Other endovascular surgery procedures, such as key-hole surgery (performed through very small incisions) and robotic procedures (performed with the aid of a moving mechanical device), increasingly are being used.
Risk stratification is of the utmost importance for identifying vulnerable patients. Specifically, pre-existing cerebrovascular disease and atherosclerosis of the ascending aorta are major determinants of the risk of peri-operative stroke, and should be always carefully scrutinised. RCTs and meta-analysis do not clearly support routine implementation of offpump CABG as a strategy to minimise the risk of stroke. Observational studies have suggested that anaortic approaches might reduce the risk of stroke compared with conventional CABG in patients with severe atherosclerosis of the ascending aorta. Further randomised controlled trials are warranted to confirm this hypothesis.
Heart stenting is another option for treating patients with CABG. The clinical application of drug-eluting stents (DES) or coronary artery bypass grafting (CABG) for unprotected left main coronary artery disease (ULMCAD) is still controversial. The need for repeat revascularization is significantly lower with CABG, but the risk of stroke is significantly higher, a trade-off that must be taken into account when considering heart stenting for patients with advanced coronary disease.
Monday, 18 August 2014
The evolution of embolic protection devices
Manipulation of atherosclerotic lesions with wires, catheters, balloons, stents and other intravascular devices during invasive procedures releases are associated with small, but clinically important and discrepant, rates of procedural complications, including cerebral and myocardial ischaemic events, cranial
nerve injury and access site haematoma. Embolic protection devices (EPDs) may lower the rate of ipsilateral ischaemic events during CAS and are considered by the majority of interventionists to be mandatory during CAS. Embolic protectiondevices can be divided into three distinct types based on their mechanism of
operation: distal occlusion aspiration devices, distal filters and proximal occlusion aspiration devices.
The importance of these devices are discussed in articles on Radcliffe Cardiology’s website, home to a number of cardiology review journals including Interventional Cardiology Review, European Cardiology Review and Arrythmia & Electrophysiology Review. Current evidence suggests improved stroke and death outcomes in contemporary series evaluation proximal EPDs compared with earlier series employing filter-type protection. The use of EPDs has been shown to substantially reduce the risk of major adverse cardiovascular events in patients undergoing saphenous vein graft (SVG) and percutaneous coronary intervention (PCI) although the actual use of
these devices in the real-world is surprisingly low. EPDs are used routinely for carotid stenting and being tested for peripheral and renal artery interventions.
Heart electrophysiology procedures which require catheters threaded to the heart also place patients at risk of embolisms. Invasive management of heart rhythm disorders by heart electrophysiology procedures including catheter ablation and device implantation has been established as the therapy of choice for most cardiac arrhythmias, and the number of patients and complex procedures has increased dramatically. An important way to promote quality in these procedures is by increasing public awareness about the
importance of heart rhythm disorders. This in turn often results in increasing public resources to reduce the impact of heart rhythm disease on society.
Wednesday, 13 August 2014
The importance of Fractional Flow Reserve (FFR) in Coronary Artery Disease Management
By Unknown00:02Cardiac Catheterization, Cardiology Conferences, Fractional Flow Reserve (Ffr)No comments

Patients with insufficient oxygen supply to the heart, or myocardial ischemia, may benefit from coronary intervention (PCI), such as stenting of partially occluded vessels. The course of treatment for patients with CAD depends on disease severity. While coronary angiography is always performed prior to PCI, it may underestimate or overestimate the severity of specific cardiac lesions. In contrast, Fractional Flow Reserve (FFR) provides a quantitative ratio of the actual blood flow in a narrowed artery, compared with the normal achievable blood flow and is more accurate in diagnosing ischemic lesions than angiography alone. Using this functional or morphological measurement, Fractional Flow Reserve (FFR) can quantify the severity of specific stenoses.
A 2012 report prepared by multiple cardiology medical societies addressed the use of FFR in appropriate use criteria for diagnostic cardiac catheterization. These appropriate use criteria recommend FFR for diagnostic evaluation of most CAD cases determined by angiography to be of intermediate, obstructive/significant or indeterminate severity. Further targeted
appropriate use criteria update for coronary revascularization were launched in the same year by various societies including the ACCF, SCAI, STS, AATS, AHA, ASNC, HFSA and SCCT. Within the criteria, the use of diagnostic cardiac catheterization
is recommended as an additional invasive measurement to determine the need for PCI for patients with coronary narrowing of uncertain severity.
The critical role of physiological fractional flow reserve (FFR), in guiding interventions is discussed at a number of cardiology conferences. One such cardiology conference is the European Society of Cardiology (ESC) 2014 which takes place in Barcelona this year. The ESC
hosts the world’s largest and most influential cardiovascular event every year in August. Record numbers of hot line sessions and abstracts were submitted this year and the congress is on track to host the largest number of delegates in its history.
Wednesday, 6 August 2014
Advances in mitral valve disease treatment
Treatment of mitral valve disease is a very common condition, affecting about 3% of the population. Recent years have seen major advances in minimally invasive mitral valve surgery and several new catheter-based techniques are being clinically evaluated. Indeed, percutaneous therapy has emerged as an option for treatment of mitral valve disease including regurgitation and prolapse for selected, predominantly high-risk patients.
Many patients with symptomatic, severe mitral regurgitation never undergo surgery due to a deemed excessive surgical risk and complete endovascular surgery is therefore an exciting alternative for these patients. Several technologies are being investigated, most of them based on long-standing surgical techniques. Over 1,000 patients have been treated worldwide with the Mitraclip system for leaflet plication, for example. This device has gained the CE mark and there has been a shift in the spectrum of candidates suitable for this technique, as recent experiences have shown that adverse mitral anatomies and functional MR patients may also benefit from this form of complete endovascular surgery and device.
An overview of recent technology for mitral heart disease can be found on Radcliffe Cardiology’s website which has a strong focus on cardiologist education. Anatomic evaluation seems crucial in order to select the most suitable patient for the procedure and cardiac computed tomography angiography is probably the best tool for patient selection. Indeed, mitral regurgitation is a complex disease with many aetiologies and pathophysiologies and therefore it seems unlikely that a single device can fix the problem. The first challenge is in fact to really understand MV disease which is why focus on education for cardiologists is so important, then a combination of techniques will be necessary for a
satisfactory MR repair. Close collaboration between interventional cardiologists, cardiac surgeons, imaging cardiologists, basic scientists and the industry is essential for these technologies to progress and become a real alternative for this group of patients.
Wednesday, 30 July 2014
Advances in valve replacement
Aortic valve replacement is becoming more common with almost 5,000 aortic valve replacements being carried
out on the NHS in England between April 2011 and April 2012. Transcatheter aortic valve implantation (TAVI) is an established alternative to surgical valve replacement in the management of calcified severe aortic stenosis in those with co-morbidities or adverse features (advanced age, impaired left ventricular function), or in those where open surgery may be associated with unfavourable technical features, such as previous sternotomy with a patent internal mammary graft, porcelain aorta or previous thoracic radiation, rendering the operative field hostile. A large body of experience and evidence exists predominantly for two commonly used TAVI devices; namely the balloon-expandable Edwards Sapien Valve (ESV) (Edwards Lifesciences Ltd, Irvine, California, US) and the self-expanding Medtronic
CoreValve (MCV) (Medtronic Inc, Minneapolis, Minnesota, US). Although the fundamental principle behind the two valves is similar, both involving a stent with three bioprosthetic cusps (leaflets) deployed within a calcified native aortic valve, the specific design features and potential indications are different. That said, studies have not shown a difference in mortality between the two valve types.
Patients may undergo cardiac catheterizationn to confirm a diagnosis of heart disease as well as treating and replacing a faulty valve.Whilst it can seem a daunting procedure for patients, it’s reassuring for them to know that cardiac catheterization has been around since the early 1940s with the advent of catheter-based interventions, pioneered by Andreas Gruentzig in the late 1970s. Since then, there has been considerable progress in the refinement and expansion of these techniques.
Continuing Education is important to keep physicians up to speed in the ever-changing world of invasive and non-invasive cardiac techniques. With this in mind Radcliffe Cardiology’s website is a good source of information for continuing education and includes many articles as well as round table discussions on TAVI and other procedures.
Thursday, 17 July 2014
Drug-eluting balloons more successful than other treament in coronary restenosis
Drug-Eluting Balloons (DEBs) are conventional semi-compliant angioplasty balloons covered with an antirestenotic drug which is released into the vessel wall during inflation of the balloon, usually at nominal pressures with a specific minimal inflation time. The active substance on the Drug-Eluting Balloons should be lipophilic enough to have a high absorption rate through the vessel wall to compensate for the short period of contact between the inflated balloon and the vessel wall itself, and to maintain a sustained effect once released.
Percutaneous treatment of complex coronary lesions, such as small-vessel heart disease, diabetes and long diffuse disease, remain hampered by suboptimal results, even with the use of drug-eluting stents (DES). The DEB is an interesting emerging device in the field of heart disease that
optimises clinical outcomes in these specific lesions. The DEB may become a viable alternative treatment option for the inhibition of coronary restenosis and subsequent revascularisation, as it allows local release of a high-concentration antirestenotic drug, paclitaxel, into the coronary vessel without using a metal scaffold or durable polymers.
Several studies have already shown promising and consistent results in the treatment of in-stent restenosis. The DEB has demonstrated its added value compared with certain DES. Inspired by these results, an increasing number of studies have been started in different coronary lesion subsets to explore the value of the
DEB in a broader range of lesions. It will be interesting for cardiology associates to see whether the DEB will find more indications beyond in-stent restenosis treatment. Moreover, will all DEBs offer the same added value, or will there be differences in efficacy among the DEBs produced by the various manufacturers? As was the case in the development of DES, now the puzzle pieces have to be put together for DEB. Potentially more good news on the horizon for cardiology associates.
Thursday, 10 July 2014
Safer alternatives to conventional coronary artery bypass (CCAB)
By Unknown00:55Cardiology Specialties, Coronary Artery Bypass Graft, Electrophysiology JournalNo comments

Adverse clinical consequences associated with conventional coronary artery bypass graft
surgery have largely been attributed to cardiopulmonary bypass circuit (CPB), hypothermic cardiac arrest, aortic cannulation and cross-clamping. Since the introduction of OPCAB for coronary artery disease, numerous studies have been published to evaluate the impact of OPCAB surgery compared with conventional coronary artery bypass graft surgery. However, subsequent prospective randomised studies and meta-analyses comparing OPCAB and CCAB surgery were performed on low-risk patients or mixed-risk populations. Due to underpowered design for infrequent complications, they usually failed to demonstrate a significant benefit of OPCAB surgery on early mortality and peri-operative major cardiac and cerebrovascular events. In recent years, further efforts have been made to elucidate the meaning of beating-heart concepts
for patients with specific extra-cardiac and cardiac risk factors for extracorporeal circulation and cardioplegic arrest.
Several mono-
and multicentre studies are currently available for patients with specific cardiac or extra-cardiac co-morbidities. Even if most of them were non-randomised and thus failed to reach American Heart Association (AHA)/American College of Cardiology (ACC) evidence level A, they still allow analysis of interim results for each specific peri-operative risk factor and help to shed light on these cardiology specialties. Particularly multi-risk patients and patients with severely reduced left ventricular function seem to benefit in terms of peri-operative mortality and major morbidity by avoiding cardiopulmonary bypass and cardioplegic arrest. Moreover, for most patients with significant extra-cardiac risk factors
the incidence of peri-operative stroke was reduced. Further insight into these cardiology specialties and risk factors are evident in European Cardiology Review, 2007;3(1):126-128.
For those looking for information on electrophysiology, sister electrophysiology journal Arrhythmia & Electrophysiology Review (AER) is a good source of information. The lastest volume 3, Issue one, includes current recommendations for cardiac resynchronisation therapy to the ablation of arrhythmias in adult congenital heart disease. This electrophysiology journal is tri-annual, helping time-pressured general and specialist cardiologists to stay abreast of key advances and opinion in the arrhythmia and electrophysiology sphere.