Continuing Education
Get Cardiology related Articles, Journals, Videos and more details at Radcliffe Cardiology site.
Online Cardiovascular Disease
Go to read Online Cardiovascular Disease relarted articles via atrial fibrillation association afa.
Cardiology Mayo Clinic
Cardiology Mayo Clinic provides informative info about cardiology at RC site.
Cardiovascular Research Foundation
Free and register PDF and journales available at here!!!
Cardiology Video
Arrange seminar and online video conference by expert cardiologist, Visit at site.
Monday, 8 December 2014
Use of Drug-Eluting Stents during Percutaneous Coronary Intervention
By Unknown01:44Coronary Fractional Flow Reserve, Cre8, Percutaneous Coronary InterventionNo comments

Narrowing of arteries and obstruction in the blood supply to the heart may lead to major cardiovascular events such as ischemia, myocardial infarction (heart attack), stroke and more. Plaques that build-up in the coronary arteries can behave in different ways: a plaque that grows to certain size and stops, a plaque that eventually causes blockage or a plaque that suddenly ruptures causing a complete block of blood supply. Chest pain during exertion is a sign of stable plaque whereas heart attack or stroke occurs when there is a plaque rupture. Cardiologists will either opt for drug therapy or revascularization procedures - percutaneous coronary intervention and Coronary Artery bypass Grafting - depending on the diagnostic results of CAD patients.
Physicians often prefer a less invasive approach as it cuts down the complications and speeds up the recovery time. Percutaneous coronary intervention (PCI), also known as coronary angioplasty have become one of the most preferred coronary interventions because of its improved outcomes and dramatic reduction of major adverse cardiac events (MACE). The procedure mainly involves widening of the narrowed artery with an inflated balloon-tipped catheter thereby restoring the normal blood flow. However, in some cases it may be essential to perform a stenting procedure to keep the arteries open. An interventional cardiologist has to take the decision about whether or not to place the stents, based on angiographic data and fractional flow reserve measurements. Coronary Fractional Flow Reserve technique used during catheterization provides a lesion-specific index that guides the physician to decide the treatment approach. Stents are placed only when the measured FFR value is less than 0.75, otherwise the patient is prescribed with medical therapy.
The well-validated and threshold value provided by the coronary fractional flow reserve technique have become a standard and reliable way to demonstrate or exclude ischemia-inducing lesions. To return to the subject of stenting, two classes of stents namely Bare-metal stents (BMS) and Drug-Eluting Stents (DES) are available for PCI. DES has superseded the use of BMS as it prevents the formation of scar tissue thereby reducing the likelihood of restenosis to a greater extent. For instance, Cre8™ DES (a polymer-free DES coated with Amphilimus™) is a new step in DES technology that overcomes the polymer-associated complications and minimises the risk of thrombosis. The amphicilic carrier present in Cre8™ DES proposes a controlled and directed drug elution. Dramatic development of nanotechnology and DES technology offers a promising approach in developing a biocompatible stent that would completely eliminate restenosis and thrombosis in near future.
Wednesday, 3 December 2014
Why Diagnosis of Treatment Resistant Hypertension is Important?
By Unknown23:02Blood Flow Blood Pressure, Treatment Resistant Hypertension, Xper Flex CardioNo comments

It is a well known fact that heart diseases have been claiming the lives of people more than any other disease. Termed as Coronary Heart Disease, this cardiac condition leads to heart attack, stroke and other major cardiovascular events. Treatment of coronary heart disease mainly focuses on controlling the risk factors by making lifestyle changes and prescribing drug treatments. High blood pressure (hypertension) and high blood cholesterol levels are the biggest risk factors that need to be brought under control. Several studies, clinical trials and research findings have stated that patients with resistant hypertension are even at higher risk of cardiovascular morbidity, stroke and mortality. Treatment resistant hypertension is a medical condition when the blood pressure remains stubbornly above the target in spite of the use of a diuretic and at least two other medications; patients whose blood pressure is controlled by four or more medications can be termed as resistant to treatment.
Accurate diagnosis and effective use of multiple drug regimens is significant in order to tackle treatment resistant hypertension. The goal blood pressure is less than 140/90 mmHg and achieving this level is even more important among resistant hypertension patients as it is associated with worse cardiovascular events. Taking accurate measurements of blood flow blood pressure is substantial for confirming treatment resistance. Direct (invasive) and indirect (non-invasive) methods are available for measuring the blood pressure and blood flow. Direct method involves using intra-arterial catheter to puncture a blood vessel and taking measurements directly, whereas the non-invasive method is about measuring the arterial pressure indirectly with a manual sphygmomanometer or an automated oscillometric device.
Physicians often prefer the indirect method because it’s the ‘gold standard’ method for routine measurements and monitoring. However, the accuracy levels of indirect measurements are low when compared to the direct methods. That is why it is important to have a hemodynamic monitoring system especially during the invasive procedures. Xper Flex Cardio physiomonitoring system introduced by Philips Healthcare is an innovative step towards this direction. It not only displays the invasive blood pressure blood flow, but also Fractional Flow Reserve measurements, ECG, respiration and other vital signs. Xper Flex Cardio systems prove to be of great use in areas where hemodynamic cardiac monitoring is required. To return to the subject of treatment resistant hypertension, we can say that ruling out the pseudoresistance factors and identification of the true causes can help in devising an effective prevention and management strategy of this condition.
Wednesday, 26 November 2014
Why FFR-Guided Revascularization Strategy Is More Effective?
Coronary Artery Disease (CAD) or Coronary Heart disease is a serious heart condition that occurs as a result of atherosclerosis. Hardening or narrowing of the artery (stenosis) causes an obstruction in the blood flow to the heart which may lead to major cardiovascular events. When the heart muscle is starved of oxygen, it results in acute chest pain and discomfort (angina) whereas heart attack (myocardial infarction) is the outcome of a completely blocked blood flow through a coronary artery. Hence, it is important to diagnose and treat coronary heart disease as early as possible, as time plays a crucial role here. Plaque build-ups along the inner walls of blood vessels can cause blockage in either single or multiple coronary arteries. Multi vessel disease (MVD) or Multi vessel CAD is the condition where a major epicardial vessel is affected with 70% or greater stenosis and other major vessels are affected with 50% or greater stenosis.
Medical therapy, Percutaneous Coronary Intervention (angioplasty and stenting) and Coronary Artery Bypass Grafting (CABG) are the treatment options available for coronary heart disease. Interventional cardiologists used to rely on angiography results and other clinical information to detect the evidence of inducible ischemia and guide treatment decisions. Notwithstanding coronary angiography is considered as the gold standard for CAD evaluation, it has been recognised to have several limitations in assessing the functional significance of coronary lesions. In the case of multi vessel coronary disease, the decision-making is far more challenging as angiographic data tend to either overestimate or underestimate the functional severity of stenosis. Revascularization of non-ischemic lesions not only increases the treatment costs but also poses an increased risk for the CAD patient rather than offering any benefit. That is when the results published by the FAME (Fractional Flow Flow Reserve versus Angiography in Multivessel Evaluation) study gained substantial interest in the medical community. It demonstrated that FFR-guided PCI can ensure better outcomes when compared to the angiography-guided PCI.
Fractional Flow Reserve (FFR) measurements can be taken easily during the invasive procedure just before the stenting. A 0.75 cut-off value helps in differentiating between ischemic and non ischemic stenosis. Lesions with a FFR value of less than 0.75 needs drug-eluting stents (DES) while lesions with a FFR value greater than 0.80 should be treated with medical therapy. The FAME study results proved that routine measurements of FFR during PCI significantly reduced the occurrence of myocardial infarction (MI), combined end point of death and repeat revascularization. So it can be hypothesised that FFR measurements are helpful in guiding decisions regarding whether CABG, stenting or medical therapy would be the optimal approach for each CAD patient.
Monday, 24 November 2014
Why Timely Coronary Artery Disease Treatment is Crucial?
By Unknown00:18Coronary Artery Disease Treatment, Coronary Artery Stenosis, Index of Microvascular Resistance2 comments

Heart muscle needs oxygen and nutrient rich blood to function properly and it is supplied by coronary arteries. When healthy, the coronary arteries remain strong, elastic and flexible which ensures the blood flow without any restrictions. However, the arterial health is compromised in some situations because of an underlying pathologic process called atherosclerosis which results in the thickening, loss of elasticity and calcification of coronary arteries. So build up of plaques in the coronary arteries coronary artery stenosis obstructs the blood flow to the heart, thereby weakening or damaging the heart muscles and this condition is termed as coronary heart disease or coronary artery stenosis disease (CAD). Whenever there is a partial blockage in blood supply, it leads to angina (chest pain or discomfort), while a complete blockage of blood flow causes myocardial infarction (heart attack).
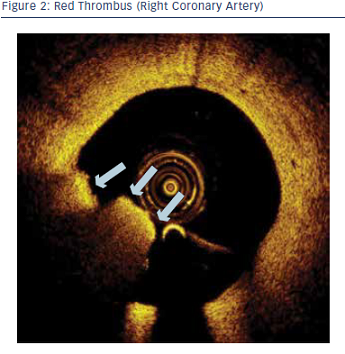
Coronary Artery Disease treatment mainly includes medications, procedures and surgeries. Even some lifestyle changes can improve the quality of life. Medications are prescribed to treat the risk factors such as blood pressures, diabetes or high cholesterol levels so that it prevents the CAD from getting worse. Surgical options include angioplasty and stenting (Percutaneous Coronary Intervention) or coronary artery disease treatment or Bypass Grafting (CABG). Depending on the severity of coronary lesions, an appropriate treatment plan is chosen by the cardiologist. Several advanced catheterization procedures and imaging techniques guide the interventional cardiologists to assess the physiological significance of lesions. Angiography, Fractional Flow Reserve (FFR), Intra Vascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT) are some of the indispensable tools used in the catheterization laboratory.
Another heart disease that has gained considerable interest in the medical community is coronary microvascular disease (CMD), which particularly occurs in women. Damage or inflammation of the inner walls of the heart’s tiny arteries is the cause of CMD. Though the presence of this dysfunction can have prognostic implications in many heart vv diseases, there are no reliable standard tests available to detect this micrhovascular disease. Diagnostic techniques developed for CAD can’t be used to assess the microvasculature of the myocardium. For now, index of microvascular resistance (IMR) is a method to investigate the microvascular integrity and functional status of micro circulation. So, FFR and IMR measurements taken simultaneously during the catheterization can help in assessing the coronary artery disease and coronary microvascular resistance disease.
Thursday, 20 November 2014
Stenting and Bypass Surgery for Patients with Left Main Coronary Artery Disease
By Unknown22:00Coronary Arterial Stenosis, Left Main Coronary Artery (LMCA), Optical Coherence Tomography (OCT)No comments

The heart is a fist-sized powerhouse that pumps oxygen and nutrient-rich blood throughout the body to keep us alive. Aorta that bifurcate into two major coronary arteries – Left Main Coronary Artery (LMCA) and Right Coronary Artery (RCA) supply blood to the heart tissues keeping them nourished so that they can function perfectly. Left Coronary Artery also known as Left main stem coronary artery (LMS) branches into Left Anterior Descending Artery (LAD) and Left Circumflex Artery that supplies the left side of the heart muscles and front of the septum with blood. While the Right Coronary Artery divides into the Right Marginal Artery and Posterior Descending Artery which supplies blood to the right side of the heart and sinoatrial nodes. Hence, any blockage in the coronary arteries will disrupt or cut off the blood flow to the heart muscles (myocardium), resulting in its damage or death.
Plaque that builds up in the coronary arteries as a result of atherosclerotic condition is the major cause of restricted blood flow. Coronary arterial stenosis of greater than or equal to 50% narrowing is associated with multivessel disease and is termed as the significant left main disease (LMD). Patients with coronary heart disease often suffer from severe chest pain and discomfort as the heart becomes starved of oxygen and nutrients. In some cases, whenever there is a clogging in the right or left main coronary artery, the collateral vessels become active, and bypassing the blockage they serve as alternative conduits for blood flow. However, it is not a cure or standard medical care option to rely on the functioning of collateral arteries.
Medical therapy and surgical revascularization (Coronary Artery Bypass Graft Surgery and Percutaneous Coronary Intervention) are the main options available for treating coronary arterial stenosis. Medical therapy was not proven beneficial for treating LMD as the survival rates were far below. Performing bare-metal stenting often ended up in higher restenosis rates, acute thrombosis and repeat revascularization. Hence, Bypass surgery (CABG) turned out to be the standard of care for left main disease as it improves the likelihood of survival.
However, advancements in catheterization and medical imaging techniques such as FFR and Optical Coherence Tomography (OCT) have led to the resurgence of interest in Percutaneous coronary Intervention (PCI). Providing a detailed and clear visualization of coronary morphology, OCT has evolved as an indispensable tool for developing new types of coronary stents. Optical Coherence Tomography when used as a guide for coronary interventions ensures better outcomes. Even though, CABG remains to be the superior choice for treating left main CAD, cardiologists hope that the ongoing studies and trials may bring more light into the role of percutaneous approach in near future.